Shoulders: Managing the Pain
Articles abound on the newer treatments for shoulder pain, creating significant confusion especially for those with complex shoulder problems and disabilities that require upper extremity use for mobility, using crutches or a wheelchair. This certainly is a concern for many polio survivors. This article follows up on a prior article written for polio survivors several years ago which includes discussion of anatomy and some specifics on causes of shoulder pain.
I would like to engage the issue of how to reason through what appears to be a maze of certain options. For anyone who has read my earlier articles on this topic (Shoulder Problems in Polio Survivors and Concepts of Shoulder Self-Management for the Polio Survivor), my approach is typically one of addressing the basics first. I firmly believe that this is essential when it comes to shoulder pain and its treatment. While there are new treatments including Biologics and shoulder surgery there is no question that these do not replace basic rehabilitation approaches, but rather augment them.
Unfortunately, there is a phenomenon of “when you have a hammer everything looks like a nail” and some providers will tend to jump to more advanced treatments and skip over the basics. Certainly, Biologics before surgery should not be excluded from treatment options for those of complex issues, but I would advise a slow approach that includes discussion with the provider that can expertly talked about a spectrum of approaches rather than just one.
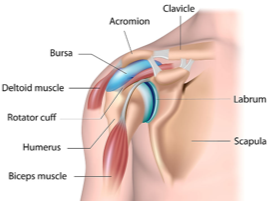
My prior article explained the biomechanics of the shoulder which includes a rather shallow cup (“the articular surface”) and ball (“the humeral head”). Without exception, the muscular and soft tissue stabilization of this joint impact pain and function regardless of the management and/or surgical approach. While some individuals may have severe arthritis with degeneration of the joint surface, impingement, tendinitis and/or bursitis are almost always contributing factors as well. Conservative treatment including anti-inflammatory medications, judicious strengthening exercises and addressing posture are foundational to any treatment plan. The anatomy of the shoulder blade and upper arm articulation creates a dynamic scenario in which a hunched posture (for example kyphoscoliosis) greatly impacts impingement of the rotator cuff with resultant inflammation and pain. Without addressing these factors other treatments may be partially successful, however future injury and/or cuff tear is still at high risk.
I have outlined some thoughts as I reason through shoulder problems and polio survivors.
Be sure the problem is actually the shoulder joint and not a separate issue referring pain to the shoulder area
a. Myofascial (muscle) pain
b. Traumatic injury/fracture
c. Referred spine pain
d. Nerve entrapment
2. Address postural concerns that result in the shoulder tipping forward
a. Consider physical therapy evaluation
b. Consider evaluation of wheelchair or sitting at home that is routinely used (a good lumbar support is important to facilitate a normal “S shape” spine and prevent a “C-shaped” kyphosis).
3. Avoid overuse
a. Minimize overhead reaching/rearrange environment if needed
b. Avoid prolonged wheelchair propulsion when fatigued. Accept assistance prior to onset of pain rather than after.
c. Consider power mobility when needed for longer distances.
d. Remember that activities that cause pain that continue after the activity are in all likelihood doing damage and can result in long-term consequences and the shoulder.
4. Consider judicious exercise
a. Consider physical therapy for education about:
Use of Thera-Band
Isometric exercises
Gentle but consistent approach remembering “an ounce of prevention is worth a pound of cure”.
b. Learning about the biomechanics of the shoulder and how strengthening the external rotator muscles reduces impingement (these are the only muscles that actually pull the humeral head down, away from the acromion and create more space for the rotator cuff).
5. Consider anti-inflammatory approaches
a. Icing for 15 minutes after activity can have an anti-inflammatory effect and thereby prevent consequences of injury from the activity. (This is commonly used by professional athletes coming off the pitching mound).
b. Over-the-counter non-steroidal anti-inflammatories. Consider regular use for 7-10 days if there are no stomach or kidney problems.
c. Consult with a physician about prescription nonsteroidal anti-inflammatories and their risks. I try to avoid long-term use in favor of 1 to 2-week bursts that serve like a “bucket of water on the fire”.
d. If the shoulder pain is debilitating, consider oral steroid medications - but remember, that due to medical risks, these should never be repeated multiple times.
e. Consider shoulder injection when advised by your physician. But, again I note that there is risk for these injections being repeated.
6. If you are considering multiple options classified as “Biologics”:
a. Further reading is highly encouraged including looking for double-blind control studies or studies that provide a “meta analysis” (summarizing multiple other studies). This article would be an example:
Effectiveness of Biologics in Shoulder Pain
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5366381/
b. Biologics options include, but are not limited to the following:
PRP (Platelet Rich Protein) injections
Growth Factor injections
Injection of Bone Marrow Aspirate/Stem Cells
Others
c. Remember that many are not covered by insurance is as there is not uniform opinion regarding the long-term benefits.
d. Remember that many products have a wide variation in how they are prepared and therefore likely also have a wide variation in efficacy (not well standardized),
e. There are some studies showing improvement in outcome however these do not offset basic rehabilitation approaches. As an example, using some Biologics along with surgical release of impingement/repair of rotator cuff can reduce the likelihood of recurrent rotator cuff tear. However, addressing any underlying issues of posture/overuse/biomechanics can certainly still have a major long-term impact on the outcome
7. Surgical options
a. Individuals with a “hook” on the undersurface of the acromion can have a dramatic reduction in impingement and reduction in the risk of rotator cuff tear, with a relatively simple surgery to remove this bony prominence area. For this reason, a surgical opinion early is often advisable as a preventative intervention rather than waiting for a full-blown cuff tear. No matter the recommendation, you can always turn it down. Information is always good, it’s what you do with it that can create problems.
b. Full rotator cuff tear surgery requires significant rehabilitation and downtime.
There is a high rate of failure if the patient returns to “overuse” too early and does not stick to the rehabilitation protocol of the surgeon.
“Prehab” (physical therapy prior to the surgery) to improve posture/shoulder biomechanics and improve strength can have improved postoperative outcome.
c. Shoulder replacement
Certainly, this is an option in those with very severe arthritis, however, there is significant risk and significant recovery/downtime.
Having a knowledgeable surgeon who understands polio-related weakness is important and can impact postoperative stability.
Be sure the surgeon has good communication skills and is fully discussing the risks. Bring a friend to advocate for you. Write down your questions/concerns in advance of the appointment.
For additional information, please read:
Concepts of Shoulder Self Management for the Polio Survivor
Shoulder Problems in Polio Survivors
In addition, I recommend these two videos.
Shoulder Anatomy Animated Tutorial by orthopod.com
I hope this information helps.