Non-Paralytic Polio Causing PPS
Back in 1949, Dr. David Bodian documented that for the poliovirus to weaken – let alone paralyze - a muscle, 60% of the motor neurons had to be killed. That means that polio survivors could have many hidden "non-paralytic" polio muscles having substantial damage but not showing symptoms. This study, published in 2022 provides more information:
Post-polio Syndrome from Non-paralytic Poliovirus Infection
Intern Med. 2022 Sep 15; 61(18): 2789–2792.
Kengo Maeda1 and Yoshiko Sugihara1:
Abstract:
“A 73-year-old man presented with muscle weakness and atrophy of his right arm. Atrophy of his left brachia and left calf had occurred 13 years before without any improvement or deterioration. His sister and cousin had a history of paralytic poliomyelitis. Serum poliovirus type 2 neutralizing antibody was elevated to 128×. Electromyography revealed chronic denervation potentials not only in the muscles affected previously but also in the unaffected muscles. Acute and chronic denervation potentials were found in the newly affected muscle. Postpolio syndrome should be considered in patients with unilateral muscular atrophy even when they have no history of paralytic poliomyelitis.”
Introduction:
“The term ‘postpolio syndrome (PPS)’ is applied to paralytic poliomyelitis survivors who develop new weakness or fatigue after achieving a long-term stable condition (1). The new weakness and atrophy affect both previously affected and unaffected muscles. Typically, these are asymmetrical or segmental (2). Polioviruses damage spinal motor neurons in the anterior horn. When the damage is less severe, paralysis is not recognized. An electromyographic (EMG) study revealed that unaffected muscles of PPS patients have large motor units as a result of effective reinnervation (3). There is a possibility that PPS may occur in people with non-paralytic polio.”
Case Report:
“Our patient was a 73-year-old Japanese man who, at 60 years old, had noticed weakness and atrophy of his left arm and calf. At that time, a blood test, including evaluations of anti-Jo-1 antibody, anti-nuclear antibody, anti-acetylcholine receptor antibody, angiotensin converting enzyme, lactate/pyruvate, vitamin B1 and B12,
anti-scl-70 antibody, and thyroid hormones, a cerebrospinal fluid (CSF) examination, and magnetic resonance imaging (MRI) of the whole spinal cord were all normal. At 69 years old, he came to our hospital complaining of persistent weakness of these muscles. The weakness had been unchanged without additional weakness for nine years. He had a family history of paralytic poliomyelitis in his sister and cousin in their childhood. He had never been abroad. No facial or bulbar palsy was found. His left deltoid, biceps and triceps brachii, and calf muscles were weak and atrophic (Fig. 1). No fasciculation was observed in those muscles. He did not show any sensory disturbances. Neither deep tendon reflexes nor pathological reflexes were elicited. A nerve conduction study (NCS) was normal. Serum neutralizing antibodies for poliovirus types 1, 2, and 3 were <4, 128×, and <4, respectively. He was thus diagnosed with PPS.”
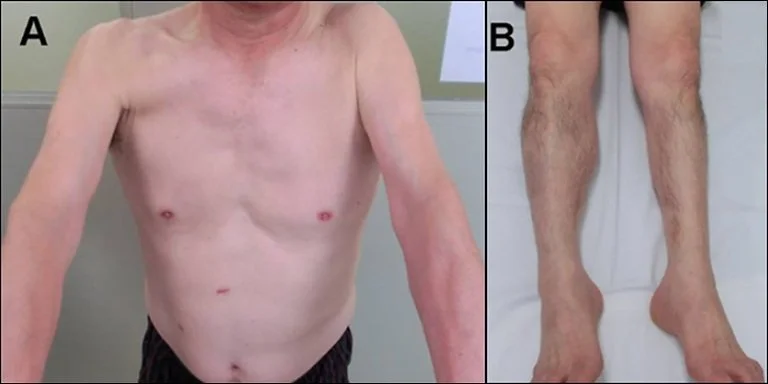
Photographs of the patient at the first visit. Muscular atrophy of
the left arm (A) and calf (B) is prominent. Photo Source.
“We simply advised him not to exercise too much. He stopped coming to our hospital until he recognized weakness of the right arm four years later.” (Summarized)
“The muscles affected previously (left deltoid and left anterior tibial) showed chronic denervation potentials, such as single oscillation of giant motor unit action potentials without acute denervation potentials.” “The unaffected right anterior tibial muscle showed acute and chronic denervation potentials, suggesting that weakness of this muscle might be ongoing.” (Summarized)
Discussion:
“Our patient had a family history of paralytic poliomyelitis affecting his sister and cousin. He has never received the oral poliovirus vaccine (OPV), nor had he ever been to polio-endemic areas. He did not suffer from acute paralytic poliomyelitis. The presence of neutralizing antibody against type 2 poliovirus suggested that he might have been infected, possibly due to close contact with his sister. Based on the clinical features, serological evidence, and EMG findings, we diagnosed him with PPS from non-paralytic polio infection.”
“ . . . PPS-like weakness or fatigue has been observed in patients with non-paralytic polio.” “PPS should be considered in patients presenting with segmental muscle weakness or atrophy with an inactive interval.”
(Summarized)
Article Source and all References: NIH – National Library of Medicine www.ncbi.nlm.nih.gov/pmc/articles/PMC9556246/
Look in the Index of the Encyclopedia of Polio and PPS for more information on the topic of “Non-Paralytic” Polio.
Non-Paralytic Polio - Additional Referenced Articles/Studies: from the NIH (National Library of Medicine)
Nonparalytic Polio and Post Polio Syndrome by Lauro Halstead, MD and Julie Silver, MD
Paralytic vs. "Nonparalytic" Polio: Distinction without a difference? by Richard L. Bruno, PhD