Insomnia (the Lack of Restful Sleep)
The First of a Multipart Series by William M. DeMayo, MD
The term Insomnia can be used in many ways. Most people would associate the term with difficulty falling asleep or difficulty staying asleep. It should also be used to describe nonrestorative sleep. Many individuals understand that there are stages of sleep yet don’t think about the fact that their quality of sleep (amount of deep sleep) is as important as their total duration of sleep. Deep sleep is essential for healing in many ways and can be seriously affected by stress/anxiety, medications, and underlying sleep disorders, such as Sleep Apnea or Periodic Leg Movement Disorder (a common variant of Restless Leg Syndrome). We will discuss these and other conditions that impair quality and quantity of sleep in future articles.
While this article will focus on the general problem of insomnia in our society, the issue is even more important for polio survivors or anyone dealing with chronic pain. Fatigue, generalized exhaustion, and pain are frequent symptoms in polio survivors, leading to suspicion of Post-polio Syndrome (PPS) but these symptoms are also seen in chronic sleep deprivation. In fact it is essential to rule out underlying sleep problems prior to assigning a diagnosis of PPS. Most people are fully aware how pain can lead to lack of sleep, but are not aware that lack of sleep will lead to pain. Lack of adequate deep sleep leads to muscle tightness/ spasm during the day, changes in our immune system’s inflammatory response, and our nervous system’s ability to regulate pain perception. Behavioral changes and medications can further exacerbate the insomnia-pain-insomnia cycle. The process of healing from minor musculoskeletal injuries is impaired without quality sleep and, over time, these unresolved “minor injuries” can become a major problem. In my practice, sleep evaluation and management is a primary focus for any patient with chronic pain, especially polio survivors.
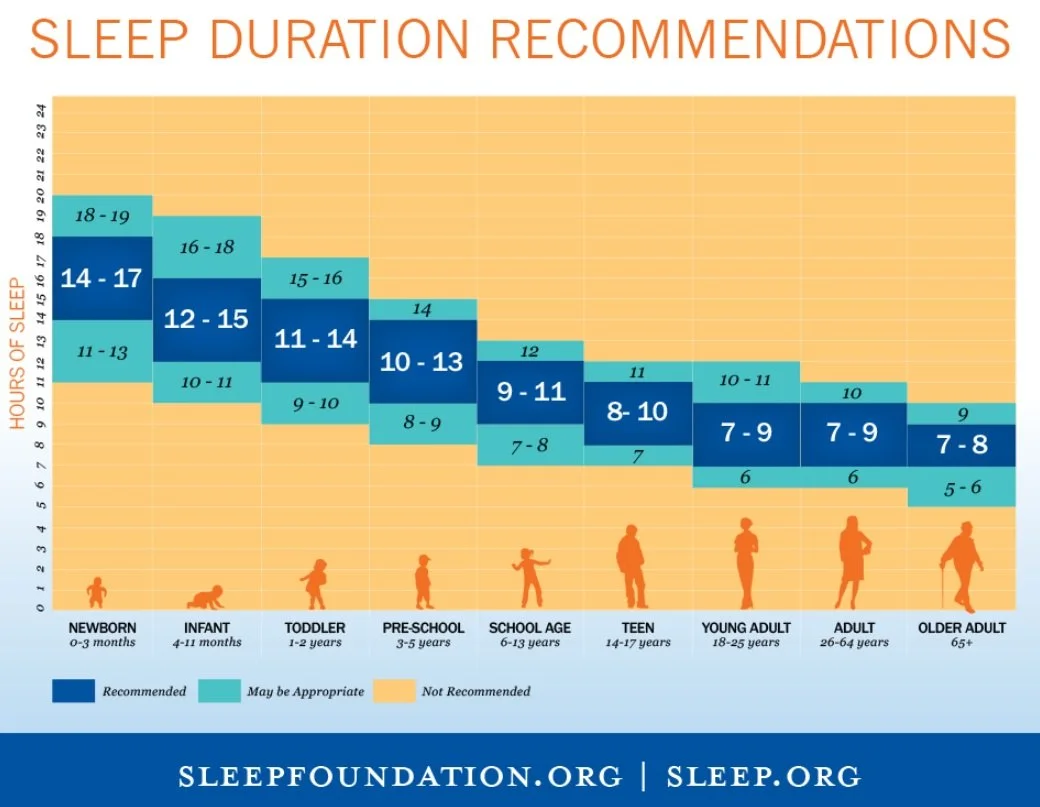
The Centers for Disease Control (CDC) reports that school-age children require at least 10 hours of sleep, teens need 9-10 hour sleep, and adults need 7-8 hours. These recommendations are similar to the national sleep foundation (see chart). Yet nearly 30% of adults reported average of less < six hours of sleep per day, and only 31% of high school students reported getting at least eight hours of sleep on the average school night. It is recognized that individual needs will vary, but the problem is most people believe that they are the exception. I thought about using an analogy with debt. I changed my mind when I saw an article about a report from the Pew Charitable Trust indicating that 80% of Americans are in debt with the median debt load being $67,900. (I mention this because it seems to be an indication that our society tends to focus on the here and now rather than the future). Instead, I will use an analogy between sleep and oil in our cars. If an individual purchases a new vehicle, there is usually an owner’s manual in the glove compartment which states the recommended number of quarts of oil to be used. If you can, imagine a friend purchasing a car and saying, “my car only needs half that amount of oil” and with the first oil change they use only half the quantity recommended. With modern engineering, the engine may start and sound as if it is working well, but anyone knows that at some point there will be a problem and the engine will either wear out early or seize up. Similarly, many people define the amount of sleep they need as being just over the amount of sleep that leads to dysfunction the next day. Most people seldom look at the long-term effect of sleep deprivation and how it can lead to “early wear” of our neurologic, cardiovascular, musculoskeletal, and immune systems.
The following statistics can be reviewed with an easy search of insomnia on WebMD. Sleep deprivation has been shown to be associated with:
Risk of accidents (100,000 auto crashes/year, 3 mile Island, Exxon Valdez oil spill, and Chernobyl have all been linked to sleep deprivation).
Impaired cognition (including decreased attention, alertness, concentration, reasoning, and problem solving).
Increased risk of serious health problems such as heart disease, heart attack, heart failure, irregular heartbeat, high blood pressure, stroke and diabetes.
Decreased libido.
Depression and anxiety.
Early aging of skin (yes, you do need your “beauty sleep”).
Memory impairments.
Weight gain. (Voluntary restriction of one hour sleep was recently correlated with a 20 pound increase in weight).
Increased risk of death.
Impairment in judgment, especially about the need for sleep. Most people think they “adapt” to the lack of sleep despite the fact that their performance on objective tests continue to decline with less sleep.
Adding to this problem, most people (including myself) are very poor at accurately reporting the quantity and quality of sleep they have experienced. As a personal example, I had a sleep study in which I remember turning over multiple times during what I thought was a three or four hour period prior to falling asleep. The actual data showed that my “Sleep Latency” was only six minutes. This was the time between when the computer showed the lights were turned out and my EEG indicated I was in stage one sleep. I only later learned that people can be quite aware of their environment when in stage one sleep. The point here is that your estimate of your sleep may be way off due to a combination of simply not paying attention and the possibility of misperception. For anyone in doubt, I would suggest a sleep diary be completed. These can be downloaded from The National Sleep Foundation (or other sources) and can provide insight about your sleep habits. Additionally, Fitbit and other activity monitors can produce computer printouts that log your sleep as well as document periods of restlessness that could indicate underlying sleep disorders. (These topics will be covered in a future article).
The focus of this first article in the series, is the old adage: “The first step in solving a problem is realizing there is one”